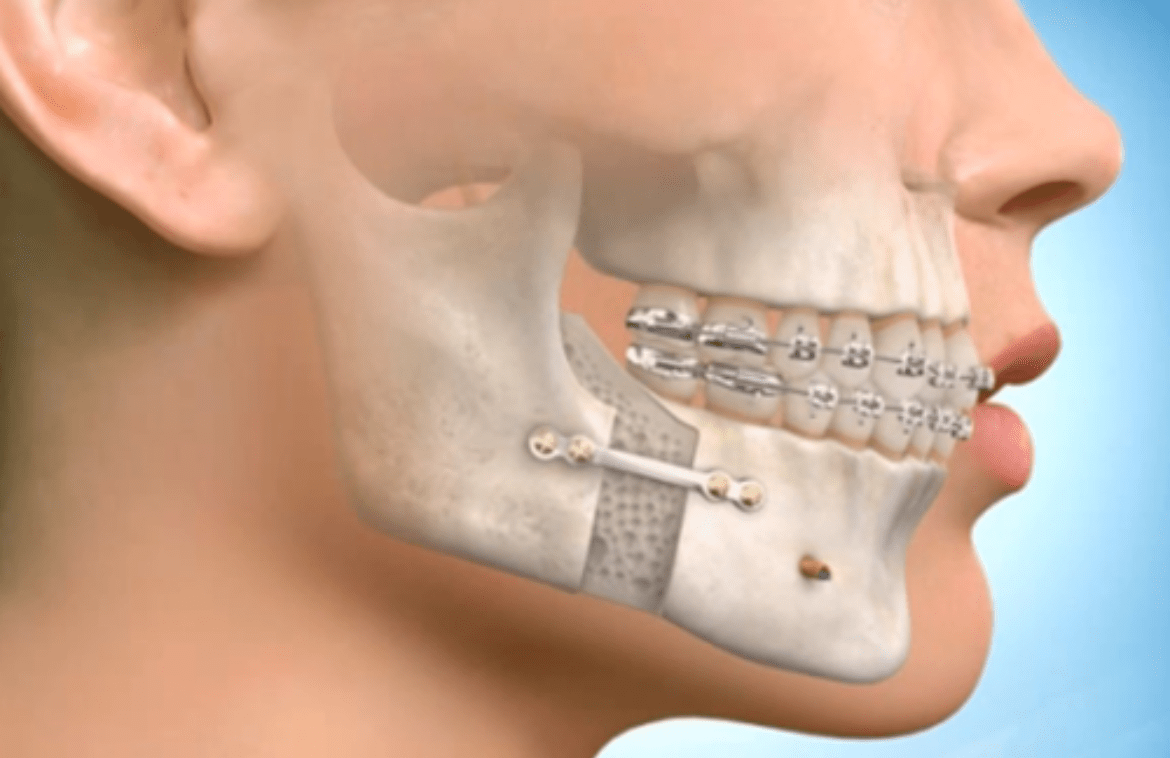
Orthognathic surgery is faced with myths and misconceptions, but it is useful to treat patients. By overcoming these orthognathic surgery myths, patients can benefit from the procedure.
Orthognathic surgery happens to be an underutilized resource in the treatment of congenital, developmental, as well as post-traumatic skeletal abnormalities in addition to obstructive sleep apnea. Despite the documented volume of patients who would indeed benefit from orthognathic surgery, most fail to really receive appropriate treatment.
Orthognathic surgery can correct malocclusions affecting a patient’s speech, function, and long-term dental health. Yet, few respondents agreed that orthognathic surgery happens to be an evidence-based treatment for obstructive sleep apnea or positively affects upper airway size.
While most dental providers do consider orthognathic surgery as an effective treatment for the surgical correction of dentofacial deformities, many tend to fail to recognize its potential role in the treatment algorithm for obstructive sleep apnea.
Orthognathic surgeries is also one of the most commonly performed facial esthetic-enhancing procedures. This could perhaps be for functional reasons, such as in severe Class III occlusion or craniofacial growth-related abnormalities like in syndromic or facial cleft patients.
Orthognathic surgery myths and about orthopedic surgeons
- Myth: They only sort of cater to professional athletes. It is true that orthopedic surgeons do help improve the fitness, health, and performance of athletes.
- Myth: All surgeons practice the same way.
- Myth: You can only find them in hospitals.
- Myth: They only perform indiscutable treatments.
- Myth: They only treat broken bones and damaged joints.
- Myth: It is not important for patients with normal occlusion who undergo orthognathic surgery to maintain their preoperative occlusal status after surgery in order to avoid orthodontic treatment, which is what patients need to believe in.
- Myth: Both dental function and aesthetic goals need not be achieved simultaneously via orthognathic surgery.
- Myth: Both dental function and aesthetic goals need not be achieved simultaneously via orthognathic surgery.
- Myth: Orthognathic surgery is not commonly performed in the field of craniofacial surgery in order to address malocclusion, problems related to the facial profile, and also obstructive sleep apnea.
- Myth: The goal of orthognathic surgery is not really to reposition the maxilla, mandible, as well as chin, and commonly performed procedures that include LeFort I osteotomy and bilateral sagittal split osteotomy (BSSO) with or without osseous genioplasty.
What more about orthognathic surgery?
Since the 1970s, orthodontic treatment has rather become popular for the treatment of malocclusion, and it has been common to combine orthodontic treatment with orthognathic surgery in order to treat both the skeletal profile as well as malocclusion.
Both dental functions as well as aesthetic goals do need to be achieved simultaneously via orthognathic surgery, and doing so does require consideration of both skeletal movement and soft tissue changes. In recent decades, the surgical goals of orthognathic surgery have, of course, shifted to become primarily aesthetic.
There are a wide variety of complications associated with orthognathic surgery, including unusual complications that are hard to predict. There should be a clear distinction between malpractice and complications. Oral and maxillofacial surgeons must have a full understanding of the types, causes, and treatment of complications and should deliver this information to patients who develop these complications. Malpractice should be avoided and is best prevented by careful and meticulous performance by surgeons.
Conclusion
Post-orthognathic surgery patient management is critical for high-quality and predictable outcomes. Surgeons and orthodontists do need the knowledge and ability to implement postsurgical management protocols and strategies to provide the best care and outcomes possible. Postsurgical orthodontic goals are to maximize the occlusal fit and also provide predictable means in order to retain the occlusion. Aggressive orthodontic mechanics may be required in order to provide the best occlusal fit. Complications can occur, but early recognition of these complications and the implementation of corrective tactics help minimize adverse outcomes.